
Osteochondrosis is one of the most common diseases of the musculoskeletal system, which manifests itself as a result of a complex of certain dystrophic changes in the spinal cartilage, during which this pathological process of the spinal discs often suffers. The structures, which are the intervertebral discs, provide flexibility as well as movement of the human spine.
Osteochondrosis involves a series of processes that cause the vertebral discs to degenerate, causing them to begin to lose elasticity and reduce the degree of flexibility, at which point the disc becomes quite flat. The distance between the two discs is reduced, while the nerve endings and blood vessels constrict and cause severe pain. The site of compression of the nerve node begins to swell, leading to increased pain and even more disruption.
Muscle structures and most organs of the body are often involved in the development of this pathological process during the development of osteochondrosis. This is due to the fact that during the maximum disruption of the neurovascular bundle, the blood circulation and movement of the muscles and organs are disrupted. For example, the most common osteochondrosis is cervical osteochondrosis, which is accompanied by pain in the head, nausea, dizziness, impaired vision, and often tinnitus. This disease was quite "rejuvenated": a century ago osteochondrosis was a disease of people of gerontological age, and today young people are also susceptible to it.

The most vulnerable category of people are those who have severely impaired metabolism and hormonal levels in the body, as well as people who have vascular-venous disorders. This is due to the fact that these diseases cause oxygen disruption of the disc. If qualified measures are not taken to heal, the edges of the affected intervertebral disc protrude anatomically beyond the boundaries of the spinal column and thus destroy the neurovascular bundle.
Because of this the patient is at risk for a herniated disc. The main, important cause of osteochondrosis is the uneven distribution of the load on the spine, which leads to the fact that the cartilage structure changes at points of excessive pressure. The nature of this disease depends on the stage and level of damage to the affected discs. The intervertebral discs change with age, as does our hair. Large injuries or fractures of the spine can affect their function. Conventional clothing and certain types of vibration can also accelerate the rate of spinal degeneration. In addition, smoking has been shown to increase the rate of spinal degeneration. The scientists also found a link between family members, highlighting the role of genetics in how rapidly changes occur.
The disease can also be caused by various factors:
- Injuries, bruises;
- Spinal muscular dystrophy;
- Spinal deviation and curvature;
- Weight gain;
- Long stay in one position;
- Metabolic disease;
- Lack of trace elements and vitamins - manganese, magnesium, zinc and vitamins D and F;
- Hereditary predisposition;
- Physical overload;
- Sedentary lifestyle;
- Radiation background;
- მოყინვა;
- Congenital dystrophies;
- Asymmetric work of the muscles of the spinal column;
- Stress, depression.
These causes of osteochondrosis are only the assumption of scientists, the direct factors that cause the disease, science has not yet found, and we are talking only about risk factors.
ᲞThe first periodDevelopment - characterized by intradiscal nucleus pulposus (eccentric intervertebral disc nucleus pulposus, early placement next to the spinal cord).
The second periodCharacterized by the manifestation of instability of the spinal segment. Pathological substrates are represented by the fibrous nucleus of the affected disc, degenerative processes of ascension, and fragmentation of the posterior longitudinal ligament, developing abnormal movements between the spines.
The third periodDevelopment of the disease - complete damage to the intervertebral disc, the appearance of a "herniated disc" - dislocation of fragments of the nucleus pulp and outside the interstitial space.
If the disease has reached the third stage, then the process of destruction is already irreversible and can lead to profound disability.
Types of osteochondrosis
The evolution of osteochondrosis is slow, with exacerbations caused by spinal injuries, exercise, weight bearing, and so on. Sh. The clinic depends on the location of the injury.
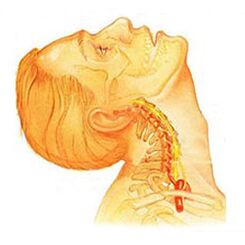
Osteochondrosis of the cervical spineHas local and distant symptoms of advanced forms - with loud domination of the roots, ie it contributes to the development of radicular acute pain. Symptoms of osteochondrosis in the cervical spine are accompanied by varying degrees of dysfunction, sometimes manifested by sudden limitations in the mobility of the cervical spine and functional blocks. The headache can be both excruciating and paroxysmal in nature, with radiation to the congenital region or the shoulder region. During the acute period, patients are diagnosed with attacks of neck pain that interfere with and restrict movement of the head and neck. In addition to acute discomfort, pain syndrome may be accompanied by dizziness, insomnia, pain, loss of appetite, depression, eye and throat diseases.

Chest osteochondrosis. . . Clinical manifestations are due to local lesions and processes of destruction of the nerve root structure. Chest osteochondrosis has a pronounced pain syndrome that may have a chronic or acute nature of back pain with discomfort in the chest and limited muscle contracture, with right verbal atrophy of the muscle. Chest pain can appear as diffuse, intercostal, and neuralgic. Palpation enhances the axial rotation of the vertebral body. Disorders correspond to the level of root irritation from Thl1 to Thl2 and may manifest as angina pectoris, which is reflected in impaired liver and gastrointestinal function. Often there is a disorder of the genitourinary system and the area around the genitals. Patients report sensory disturbances such as paresthesia, superficial and deep sensitivity significantly reduced.

Lumbar osteochondrosis. . . It is characterized by abdominal reflexes and dysfunction of the lower extremities. Muscle weakness in the legs and pelvic organ dysfunction can occur during the development of neurological disorders. Osteochondrosis is characterized by the assessment of damage to the sitting process. The more advanced the stage of lumbar spine injury, the shorter the patient sits. Lumbar forms are characterized by chronic and severe spinal pain, intervertebral muscle spasm, and myofacial secondary syndrome. The pain radiates to the buttocks and back ilium.
Depending on the localization of the pathological process of osteochondrosis, the disease can lead the patient to a disturbance of superficial sensitivity (tactile, thermal). Also characteristic are changes in reflexes (e. g. , no Achilles reflex), muscle wasting, impaired muscle tone, autonomic disorders (paleness, redness of the skin, trophic changes in the nails, skin hypothermia in the distal extremities), dysfunction of the sphincter.
Clinical picture
DiagnosisIt starts with a complete history and physical examination. The doctor asks questions about the symptoms, how the disease interferes with the patient's daily activities. Also, the specialist is interested in identifying positions and actions that emphasize or reduce the level of pain.
The doctor then examines the patient, checks the position of the spine and the range of motion, thus determining which movements are causing the pain. Skin sensitivity, muscle strength and reflexes are equally tested. Based on your medical history and physical examination, your doctor will determine which techniques will help you.
Radiographs rarely aid in diagnosis, with no more than 30% of radiographic images showing abnormalities in the early stages of disease development.
However, if the symptoms are severe and the disease is already in the second or third stage, the picture shows one or more intervertebral disc defects. Osteophytes can penetrate between the spine and the joints.
Magnetic resonance imaging is prescribed if additional information is needed. MRI is used to examine soft tissues. This is useful if the fabric core is absorbing water, or if there are cracks in the disc. MRI can show problems in other soft tissues, such as the spinal nerves.
Discography can help with the diagnosis. This test is performed using a contrast agent that is inserted into one or more disks accordingly. Further examination of the radiograph provides useful information about the condition of the discs.
Treatment of osteochondrosis, depending on the variety
Non-surgical treatment of osteochondrosis
When possible, doctors prefer non-surgical treatment. During non-surgical treatment, the most important thing is to alleviate the pain and other discomfort so that the patient can maximize a comfortable standard of living.
Doctors rarely prescribe bed rest for patients with osteochondrosis problems. Patients are encouraged to live in natural mobility when pain is not bothering them. If symptoms are severe, bed rest may be scheduled for a few days.
When moving the spine, an elastic band is sometimes prescribed, which is worn for no more than 2-4 days to prevent atrophy of the back muscles.
Osteopathic sessions seriously relieve osteochondrosis.Osteopathy doctorNot only diagnoses the problem area, but also relieves pain in 1-2 doses, relieves the general condition of the body and "tightens" the visceral organs.
Patients may be prescribed medications to control symptoms and resume normal activities for a long time. If symptoms persist to limit the patient’s activities, your doctor may usually suggest an epidural steroid injection.
Steroids are powerful anti-inflammatory drugs, helping to relieve pain and inflammation. Nonsteroidal anti-inflammatory drugs (NSAIDs) are given in the area around the spinal cord roots. This place is called the epidural space. Some doctors take steroids alone. However, it is most often combined with other drugs. Basically, steroids are prescribed only when other medications are ineffective, but osteopathy almost always helps.
In addition, patients often work with physical therapists. After assessing the patient's condition, the therapist prescribes exercises to reduce symptoms. The exercise program aims to improve flexibility and is useful for exercising the abdominal and spinal muscles to ensure movement with the least amount of pain.
Surgery
People with osteochondrosis problems usually do not need surgical treatment. In fact, only 1-3% work. Surgeries prescribe non-surgical treatment, namely craniocerebral osteopathy, as rehabilitation therapy for at least 3 months before surgery is performed. If after 3 months of non-surgical treatment there is no result, only then is there a reason to refer to the surgical procedure.
Basic surgical procedures
Discectomy
The procedure is aimed at partial or complete removal of the disc in the lumbar region. Surgeons usually perform the operation through an incision in the lumbar region. Some plates must be removed before removing the herniated disc.
Today, surgery has mastered minimally invasive techniques that require a small drop in the lumbar region. Proponents of her case have been working to make the actual transcript of this statement available online. They also believe the procedure prevents the development of scars around nerves and joints and helps patients recover faster.
Merger
It is an intervention that joins two or more bones into one, preventing the wear of bones and joint ends.
Rehabilitation
The doctor may recommend the patient to a physical therapist several times a week for 4-6 weeks. In some cases, patients need extra help.
The first year of treatment is needed to control symptoms. The therapist will work with you to find positions and movements that will ease the pain. Heat, cold, ultrasound and electrical stimulation may be prescribed to relieve pain and muscle spasm. Massage or specialized forms of soft tissue mobilization may also be used. These procedures help the patient to perform movements easily.
Typically, adjusting the treatment helps to restore the sensitivity of the spinal nerves and muscles, reduce pain, and improve mobility.
The main goal of therapy is to teach the patient how to manipulate to avoid future problems. The patient is advised to perform a series of exercises to improve flexibility. The patient will also be given a strategy to help with recurrent symptoms.
Each person should study and consider all types of osteochondrosis to prevent the development of this disease in themselves and their loved ones. Unable to treat a destroyed spine, therapy aims to alleviate pain symptoms and achieve long-term remission. You should also remember a simple but effective rule:The best remedy is prevention. . .
Prevention of osteochondrosis
Prevention is quite simple - it is a healthy diet, regular muscle activity, daily morning heating, a healthy and active lifestyle and a monthly visit.Osteopathic sessionsFor the correction and removal of muscle tension. Adherence to these rules is enough to never meet the above problem and to avoid terrible symptoms and lifelong treatment.
































